This is the story of Emma Wren Gibson, the embryo that was frozen for 24 years. The story starts on a cold October day in 1992 after an embryo was made in a laboratory. It was one of many created during early in vitro fertilization procedures. It was frozen, catalogued, and stored. For families and clinicians it was an ordinary piece of medical history. For that tiny cluster of cells, however, history would take a strange turn.
More than two decades later it would be chosen by a young couple in Tennessee, carried to term, and born as a healthy baby girl named Emma Wren Gibson. Her arrival in November 2017 made headlines precisely because of the time the embryo had spent on ice. Her birth asked unexpected questions about the limits of medicine, the meaning of parenthood, and the ethics of embryo donation.
How an embryo becomes a record
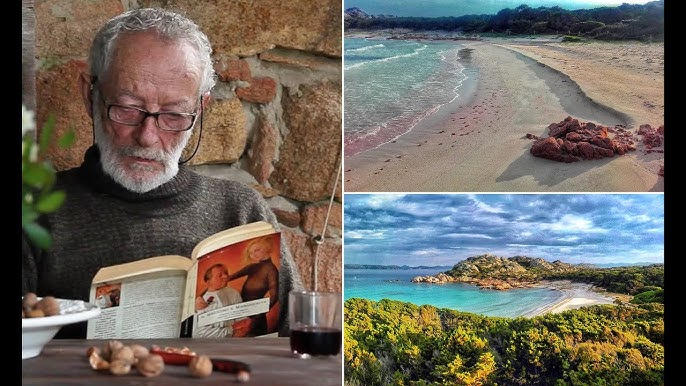
By the early 1990s, embryo freezing was part of the standard toolbox in assisted reproduction. Clinics created embryos, some would be transferred immediately, others cryopreserved for future use. Over time those stored embryos became a resource: for the original couple, for research, or for donation to other families. The embryo that would become Emma Wren was created on October 14, 1992. It remained vitrified, untouched by time, until it was chosen in 2017. When the National Embryo Donation Center in Knoxville, Tennessee, announced the birth, researchers and media flagged the case because it appeared to be the longest interval between cryopreservation and a live birth on record at that time.
The center that handled Emma’s transfer, the National Embryo Donation Center or NEDC, is a faith-based nonprofit that facilitates embryo donation and transfer. Couples or individuals choose donated embryo profiles, agree to screening and medical protocols, and proceed to transfer if a match is reached. In Emma’s case the couple who received the embryo, Tina and Benjamin Gibson, were unaware at first of how old the embryo was. Tina was born in 1991. The embryo that would become her daughter had been made a year later. That particular detail captured the public imagination: the child was conceived before the mother was born.
Tina and Ben Gibson did not become parents the moment they first considered embryo adoption. Their path involved infertility concerns in the family, foster care, searching, prayer, and eventually the deliberate decision to pursue embryo donation. Infertility is often a private struggle, and adoption choices can be guided by values, faith, finances, and medical advice. The Gibsons visited the NEDC and reviewed donor profiles. They read through dozens of options and eventually selected a donor embryo they felt right about. The embryo they chose was one of several they considered, and it became their second-choice embryo that ultimately took. The transfer occurred in March 2017 and by late November the baby was in their arms.
What the Gibsons emphasized in media interviews was gratitude. They called Emma a gift. For clinicians, the case was an example of how long embryos can remain viable under careful cryogenic storage. For people thinking about embryo donation the story became a prompt: if embryos can wait 24 years and then produce a healthy baby, perhaps others could, too.
How embryo perservation works
Cryopreservation works by cooling cells to very low temperatures so that metabolic processes stop. Modern methods such as vitrification prevent ice crystals from forming inside cells, which otherwise would damage delicate structures. When embryos are stored properly and monitoring protocols are followed, many embryologists believe embryos can remain viable for a very long time. In Emma Wren’s case the 1992 embryo had been managed under conditions that preserved integrity for decades. The embryologist associated with the transfer noted the quality of the preservation and how remarkable it was that the embryo survived thawing and implantation so many years later.
Still, saying embryos can survive indefinitely is not the same as claiming an infinite or guaranteed shelf life. Storage depends on consistent temperature control, proper record keeping, and careful handling. For clinics and patients, the Gibson story served as an affirmation of the technology, not as a promise that every embryo will always survive the wait.
Media love a good record. Headline writers christened Emma a possible world record as the longest-frozen embryo to produce a healthy birth at the time of her arrival. That description was accurate in context: research librarians and clinic records could find no older successful case in the literature then available. That said, records are provisional and new cases can emerge. Later births would surpass Emma’s interval, but at the moment of her birth the claim was newsworthy and grounded in the NEDC’s review of the medical library.
A related phrase sometimes used in stories is “snow baby.” It is a colloquial and somewhat sentimental term used by advocates and clinics for embryos in long-term storage. For families who have embryos in storage, Emma’s story brought hope; for clinicians it affirmed long-term cryopreservation as a viable reproductive tool; for ethicists it reopened debates about rights, stewardship, and the responsibilities that accompany stored embryos.
Emma’s story has multiple human threads that drew attention.
One was the emotional image that Tina offered during interviews. She joked, ruefully, that Emma could have been her friend had she been born in 1993 when Tina was a toddler. That image—of a child conceived before the mother was born—filled social feeds and made readers think about time, identity, and family in new ways. It humanized the abstract science.
Another thread was the notion of choice. The Gilsons did not randomly receive an embryo. They reviewed donor profiles, faced screening, and made a deliberate decision to accept a donated embryo. For many families embryo donation is a route to parenthood that sits between adoption of children and traditional IVF. It raises different practical and emotional questions. Would the parents tell the child later? How would they describe the donor? What are the legal and medical records that follow an embryo across decades? The Gibson family, like many who choose embryo adoption, spoke openly about gratitude and faith.
Finally there is the afterlife of medical files. The embryo had an origin with a different couple in 1992. Those donors made a choice—whether to keep embryos, destroy them, or donate them. Over time many couples choose donation to give others a chance to parent. Emma’s birth highlighted how those donor decisions can ripple forward years later.
Any headline about “the oldest frozen embryo” stirs medical curiosity and ethical debate.
From a medical perspective, clinicians asked whether long-frozen embryos raise unique pregnancy risks. The available evidence does not suggest embryos that survive thaw and implant are inherently riskier than typical IVF embryos. Outcomes hinge on maternal health, the embryo’s quality, and the standard prenatal care that follows. In Emma’s case her birth and early metrics were normal: weight, length, and immediate health indicators were within expected ranges. Clinicians involved emphasized that successful outcomes are possible even after decades of storage, provided quality control measures are in place.
From an ethical angle, embryo donation raises questions about consent, record keeping, and future intentions of donors. How do clinics maintain contact with donors across the years if a family later wants to know the embryo’s origins? What happens if documentation is incomplete? How should clinics counsel donors and recipients on the implications of long-term storage? The NEDC and similar centers address these issues with screening, informed consent processes, and donor profiles intended to give recipients some background information. Those measures are not perfect, but they are standard practice intended to respect both donor and recipient autonomy.
There are also social questions. Some critics worry about the commercialization of reproductive materials. Others raise moral objections grounded in beliefs about when life begins, or who should be able to use donated embryos. Clinics and patients navigate these debates in different ways, often guided by legal frameworks and institutional policies.
The Gibsons kept the media narrative simple. They emphasized faith, family, and the emotional relief of becoming parents. They also described practical steps: the selection of donor profiles, the medical preparation of Tina’s uterus, the thawing and transfer, and the joy of a healthy birth after months of pregnancy. They framed Emma’s birth as a personal miracle rather than a headline-chasing stunt. For them, the medical detail mattered less than the daily rhythms of parenting that followed.
The NEDC framed the story similarly. Clinic leaders used Emma’s birth to encourage conversations about embryo donation options among families who might otherwise simply discard unused embryos. The center’s public messaging mixes medical explanation and faith-based values, seeking to position embryo donation as a life-affirming option.
Emma’s birth did not occur in a vacuum. Embryo donation and adoption have expanded over the last two decades. Some couples who complete IVF cycles donate unused embryos to research, to disposal, or to other families. Organizations such as the NEDC match donors and recipients. The practice has created a community sometimes called the “snow baby” network mixed with adoption-style narratives and occasional legal complexities. Estimates suggest thousands of births have resulted from donated embryos. For prospective parents exploring options, embryo donation can be less costly than traditional IVF and more accessible than some forms of adoption. It also involves medical screening and legal paperwork.
Emma Wren Gibson’s birth matters for several reasons.
First, it is an affirmation of a technology that reliably preserves human embryos for long periods when done correctly. That knowledge shapes clinic protocols, patient counseling, and donor decisions.
Second, it humanizes abstract debates about reproductive ethics. When the topic moves from law journals to a sleeping baby in a family’s arms, the moral calculus changes. Families, donors, and clinicians must balance belief, science, and the practicalities of caring for future children.
Third, the case invites reflection on time and parenthood. Parents who adopt embryos may raise children who have no genetic link to them but have deep parent-child bonds. The fact that an embryo could predate the mother complicates simple ideas about lineage, generation, and the meaning of biological age.
Finally, the story is a reminder that advances in medicine create both opportunities and responsibilities. As preservation technology improves, clinics and regulators will face new questions about long-term storage, data, and consent.
Emma Wren Gibson’s life began in a lab in 1992 and then paused in a frozen state for 24 years. When she arrived in 2017 she became a small, ordinary citizen of a much larger story about what medicine allows humans to do with life and time. The headlines called her a record. For her family she was simply a child they had wanted more than anything. For medicine she was proof that careful preservation could bridge decades. For the public she was an invitation to think about how technology changes our understanding of family, age, and the ethical responsibilities of care.
What started as a clinical procedure became, quite literally, a life that stretched the imagination. That is why Emma’s story still matters. It is not only about what science can preserve. It is about the people who live on the other side of that preservation: donors, parents, clinicians, and the little lives that show up one November morning to rewrite our expectations.